Harvoni medication Uses, Dosage, Side Effects, Precautions & Warnings
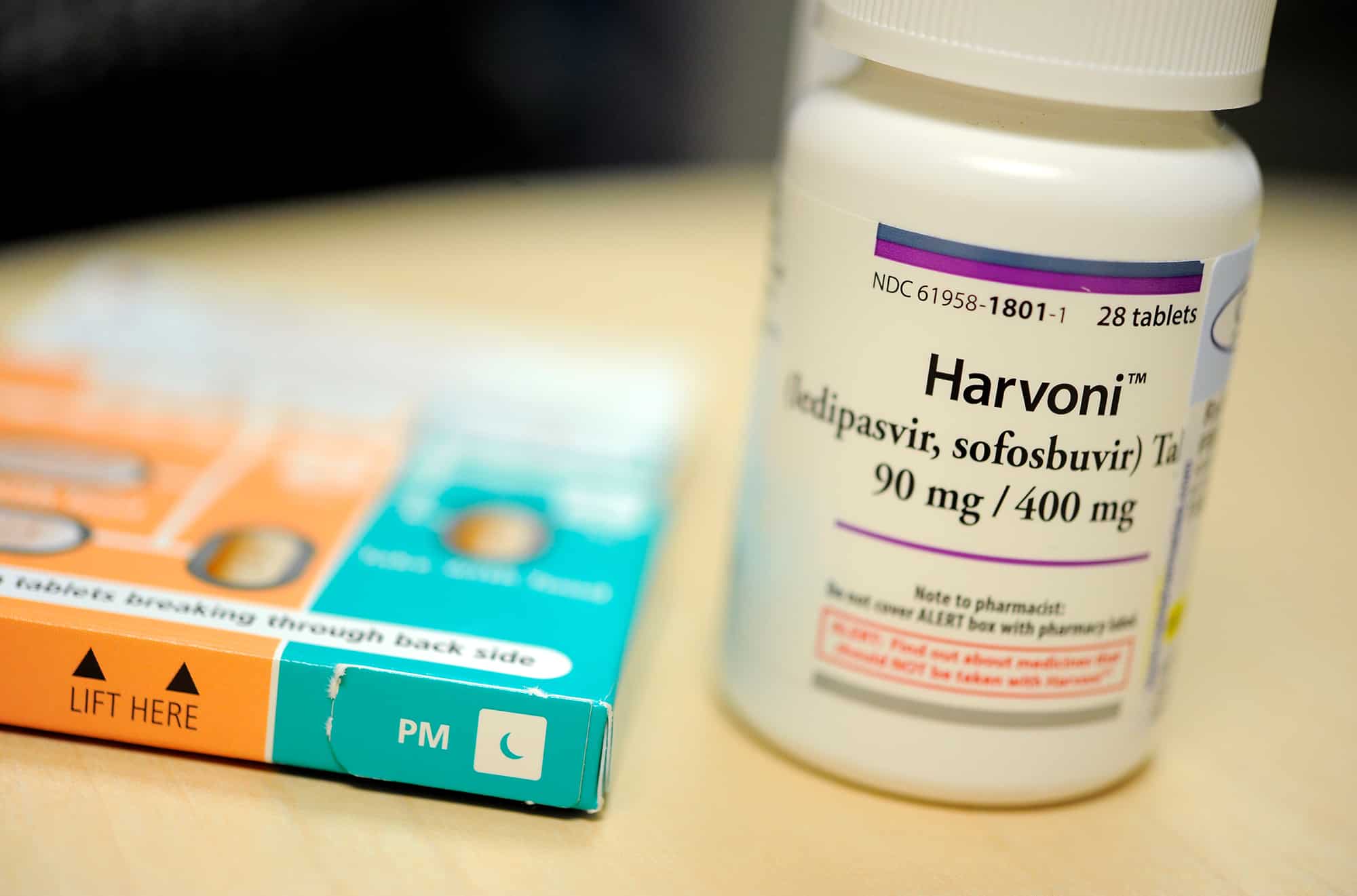
Harvoni medication >>> Generic drugof the Therapeutic class: Gastro-Entero-Hepatology
active ingredients: Ledipasvir , Sofosbuvir
Important to know about harvoni medication ?
- Sofosbuvir and ledipasvir inhibit the growth of hepatitis C virus.
- In chronic hepatitis C (liver inflammation).
- It takes several months until your symptoms decrease, such as fatigue and abdominal complaints.
- A course usually lasts 12 to 24 weeks, sometimes 8 weeks is sufficient. Complete the entire course, even if your symptoms have already disappeared.
- You may take the tablet with or without food. Swallow it whole, without chewing. The tablet tastes otherwise very bitter.
- Are you nauseous and do you have to vomit? If you have to vomit within 5 hours after swallowing this medicine, you must take a new tablet. Otherwise, it does not work properly.
- Side effects may include headache, fatigue, skin rash and hypersensitivity.
- There are many interactions with other means. Have your pharmacist check whether you can use it safely with your other medicines, even those that you have bought without a prescription.
what is harvoni used to treat and indication?
Harvoni is indicated for the treatment of chronic hepatitis C (CHC) in adults (see sections Dosage and Administration , Warnings and Precautions and Pharmacodynamic properties ).
For activity based on hepatitis C virus (HCV) genotype, see Warnings and Precautions andPharmacodynamic Properties sections .
Harvoni Dosage
Dosage
The recommended dose is one Harvoni tablet once a day, with or without food (see section Pharmacokinetic properties ).
<brarial’,’sans-serif’; color:=”” black”=””>Table 1: Recommended duration of treatment with Harvoni and recommendations for co-administration with ribavirin in certain subgroups</brarial’,’sans-serif’;>
| Patient population * | Treatment | Duration | |
| Patients with genotype 1 or genotype 4 HCC | |||
| 12 weeks.
– A duration of 8 weeks could be considered in patients infected with genotype 1 not previously treated (see section <iarial’,’sans-serif’; color:=”” black”=””>Pharmacodynamic properties, ION-3 study).</iarial’,’sans-serif’;> |
|||
| Patients without cirrhosis | Harvoni | – A duration of 24 weeks should be considered in previously treated patients for whom the possibilities of subsequent re-treatment are uncertain (see section Warnings and precautions for use ). | |
| Patients with compensated cirrhosis | Harvoni | 24 weeks.
– A duration of 12 weeks could be considered in patients for whom the risk of clinical progression of the disease is considered low and for whom subsequent retreatment options exist (see section 4.4 ). |
|
| Patients with decompensated cirrhosis or in a pre / post liver transplant situation | |||
| Harvoni + ribavirin | 24 weeks (see warnings and precautions for use and Pharmacodynamic properties ) | ||
| Patients with genotype 3 CHC | |||
| Patients with cirrhosis and / or failure of a previous treatment | |||
| Harvoni + ribavirin | 24 weeks (see warnings and precautions for use and Pharmacodynamic properties ) | ||
* Includes patients co-infected with human immunodeficiency virus (HIV).
- If used in combination with ribavirin, see also the Summary of Product Characteristics for ribavirin.
- In patients without decompensated cirrhosis and requiring the addition of ribavirin in their treatment (see table 1), the daily dose of ribavirin is calculated according to the weight (<75 kg = 1000 mg and ≥ 75 kg = 1 200 mg) and is administered orally in two divided doses, with food.
- In patients with decompensated cirrhosis, ribavirin should be administered at the starting dose of 600 mg divided over the day. If the initial dose is well tolerated, the dose may be increased gradually to a maximum of 1000-1200 mg per day (1000 mg for patients weighing <75 kg and 1200 mg for patients weighing ≥ 75 kg ).
- If the initial dose is not well tolerated, the dose should be reduced as needed based on hemoglobin levels.
Dose modification of ribavirin in patients taking 1,000-1,200 mg per day
- If Harvoni is used in combination with ribavirin and a patient experiences a serious side effect potentially related to ribavirin, the dose of ribavirin should be changed or the treatment stopped, if necessary, until the side effect disappears or its severity decreases. Table 2 gives the recommendations for dose modification and discontinuation of treatment depending on the hemoglobin concentration and the patient’s heart condition.
Table 2: Recommendations for dose modification of ribavirin co-administered with Harvoni
| Biological values | Reduce the ribavirin dose to 600 mg / day if: | Stop ribavirin if: |
| Hemoglobin levels in patients without heart disease | <10 g / dL | <8.5 g / dL |
| Hemoglobin level in patients with a history of stable heart disease | Decrease in hemoglobin ≥ 2 g / dL during a 4 week treatment period | <12 g / dL despite taking a reduced dose for 4 weeks |
- When ribavirin has been discontinued due to a biological defect or clinical manifestation, an attempt may be made to re-initiate ribavirin at a dose of 600 mg per day and then increase further. the dose up to 800 mg per day. However, increasing ribavirin to the dose initially prescribed (1000 mg to 1200 mg per day) is not recommended.
- Patients should be informed that if they vomit within 5 hours of taking their dose, they should take another tablet. If they vomit more than 5 hours after taking their dose, it is not necessary to take another dose.
- Patients should be informed that if they forget to take a dose and they notice it within 18 hours of their usual dose, they should take the tablet as soon as possible and then take the next dose as scheduled . If they find out more than 18 hours later, they should wait and take the next dose as scheduled. Patients should be instructed not to take a double dose.
The elderly
- No dose adjustment is necessary in elderly patients (see section Pharmacokinetic properties ).
Renal failure
- No dose adjustment of Harvoni is necessary in patients with mild or moderate renal impairment. The safety of ledipasvir / sofosbuvir has not been evaluated in patients with severe renal impairment (estimated glomerular filtration rate [eGFR] <30 mL / min / 1.73 m 2 ) or d end-stage renal disease (ESRD) requiring hemodialysis.
Hepatic insufficiency
- No dose adjustment of Harvoni is necessary in patients with mild, moderate or severe hepatic impairment (Child-Pugh-Turcotte score [CPT] A, B or C) (see section Pharmacokinetic properties ). The safety and efficacy of the ledipasvir / sofosbuvir combination have been established in patients with decompensated cirrhosis (see section Pharmacodynamic properties ).
Pediatric population
- The safety and efficacy of Harvoni in children and adolescents under 18 years of age have not been yet been established. No data is available.
Administration mode
Oral use.
- Patients should be informed that they should swallow the tablet whole, with or without food. Due to its bitter taste, it is recommended not to chew or crush the film-coated tablet .
what’s Contraindications for
harvoni?
- Hypersensitivity to the active ingredients or to any of the excipients listed in the Composition section .
- Co-administration with rosuvastatin or St. John’s wort ( Hypericum perforatum ) (see section Interactions with other medicinal products and other forms of interaction ).
harvoni how does it work?
Absorption
- After oral administration of ledipasvir / sofosbuvir in HCV infected patients, the median peak plasma concentration of ledipasvir was reached 4.0 hours after dosing. Sofosbuvir was rapidly absorbed and the median plasma peaks were reached ~ 1 hour after dosing.
- The median plasma peak of GS-331007 was reached 4 hours after
administration.
- Based on population pharmacokinetic analysis in HCV-infected patients, geometric means of steady-state AUC 0-24 for ledipasvir (n = 2,113), sofosbuvir (n = 1,542) and GS-331007 (n = 2,113) were 7,290, 1,320 and 12,000 ng • h / mL, respectively. The steady-state C max for ledipasvir, sofosbuvir, and GS-331007 were 323, 618 and 707 ng / mL, respectively. The AUC 0-24 and C max of sofosbuvir and GS-331007 were similar in healthy adult volunteers and in patients infected with HCV.
- Compared to healthy subjects (n = 191), AUC 0-24 and C maxof ledipasvir were 24% and 32% lower, respectively, in HCV-infected patients. The AUC of ledipasvir is dose proportional over a dose range of 3 to 100 mg.
- The AUCs of sofosbuvir and GS-331007 are quasi-dose-proportional over a dose range of 200 mg to 400 mg.
Effects of food intake
- Compared with fasting, administration of a single dose of ledipasvir / sofosbuvir with a moderate or high fat meal increased the 0-inf AUC of sofosbuvir by approximately 2-fold. but did not significantly change sofosbuvir C max .
- Exposures to GS-331007 and ledipasvir were not affected by these two types of meals. Harvoni can be administered with or without food.
Distribution
- The binding of ledipasvir to human plasma proteins is> 99.8%. After administration of a single 90 mg dose of [ 14 C] -ledipasvir in healthy subjects, the blood / plasma radioactivity ratio [ 14 C] was between 0.51 and 0.66.
- The binding of sofosbuvir to human plasma proteins is approximately 61 to 65% and the binding is independent of the concentration of the product, in the range of 1 to 20 µg / mL. The binding of GS-331007 to proteins is minimal in human plasma. Following a single 400 mg dose of [ 14 C] -sofosbuvir in healthy subjects, the ratio of blood [ 14 C] to plasma radioactivity was approximately 0.7.
Biotransformation
- In vitro, no detectable metabolism of ledipasvir by human CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6 and CYP3A4 has been observed. Evidence of slow oxidative metabolism, the mechanism of which is not known, has been observed. After administration of a single 90 mg dose of [ 14 C] -ledipasvir, systemic exposure was almost exclusively due to the parent drug (> 98%). Unchanged ledipasvir is also the main form found in faeces.
- Sofosbuvir is extensively metabolized in the liver to form the pharmacologically active nucleoside triphosphate analog GS-461203. The active metabolite is not detected. The metabolic activation pathway involves sequential hydrolysis of the carboxyl ester group, catalyzed by human cathepsin A or carboxyl esterase 1, and phosphoramidate cleavage by the HINT1 protein (histidine triad nucleotide-binding protein) followed by phosphorylation by the pyrimidine-nucleotide biosynthesis pathway. Dephosphorylation results in the formation of the nucleoside metabolite GS-331007, which cannot be re-phosphorylated effectively and which lacks anti-HCV activity in vitro. In the case of the ledipasvir / sofosbuvir combination, GS-331007 represents approximately 85% of the
Elimination
- After a single 90 mg oral dose of [ 14 C] -ledipasvir, the average total recovery of radioactivity [ 14 C] in faeces and urine was 87%, with most of the radioactivity was recovered in faeces (86%). Unchanged ledipasvir excreted in the faeces averaged 70% of the administered dose and the oxidative metabolite M19 represented 2.2% of the dose. These data suggest that the primary route of elimination for unchanged ledipasvir is biliary excretion, with renal excretion being a minor route (approximately 1%). The median terminal half-life of ledipasvir in healthy volunteers following administration of ledipasvir / sofosbuvir on an empty stomach was 47 hours.
- After administration of a single 400 mg oral dose of [ 14 C] -sofosbuvir the mean total dose recovery was greater than 92%, of which approximately 80%, 14% and 2.5% recovered in the urine. faeces and exhaled air, respectively. The majority of the sofosbuvir dose recovered in the urine was GS-331007 (78%) and 3.5% was sofosbuvir. These data show that renal clearance is the primary route of elimination for GS-331007 with a large proportion actively excreted. The median terminal half-lives of sofosbuvir and GS-331007 after administration of ledipasvir / sofosbuvir were 0.5 and 27 hours, respectively.
- Neither ledipasvir nor sofosbuvir are substrates for active hepatic transporters, organic cation transporter (OCT) 1, organic anion transporting polypeptide (OATP) 1B1 or OATP1B3. GS-331007 is not a substrate for renal transporters, including organic anion transporter (OAT) 1 or OAT3, or OCT2.
Potential in vitro effect of ledipasvir / sofosbuvir on other medicinal products At concentrations achieved in clinical practice, ledipasvir is not an inhibitor of hepatic transporters, including OATP 1B1 or 1B3, BSEP, OCT1 , OCT2, OAT1, OAT3, the transporter MATE (mutidrug and toxic compound extrusion) 1, the multidrug resistance protein (MRP) 2 or the MRP4. Sofosbuvir and GS-331007 are not inhibitors of the drug transporters P-gp, BCRP, MRP2, BSEP, OATP1B1, OATP1B3 and OCT1, and GS-331007 is not an inhibitor of OAT1, ‘OCT2 and MATE1.
Sofosbuvir and GS-331007 are not inhibitors or inducers of CYP or uridine diphosphate glucuronosyltransferase (UGT) 1A1 enzymes.
Pharmacokinetics in special populations
Ethnicity and gender
- No clinically significant pharmacokinetic differences due to ethnicity were noted for ledipasvir, sofosbuvir or GS-331007. No clinically significant pharmacokinetic differences due to gender were noted for sofosbuvir or GS-331007. The AUC and C max of ledipasvir were 77% and 58% higher, respectively, in women compared to men. However, the relationship between gender and ledipasvir exposures was not considered clinically relevant.
The elderly
- Pharmacokinetic analysis of HCV-infected patient populations showed that, in the age range analyzed (18-80 years), age has no clinically significant effect on exposure to ledipasvir, sofosbuvir or GS-331007. The clinical studies of ledipasvir / sofosbuvir included 117 patients aged 65 years and over.
Renal failure
- The pharmacokinetics of ledipasvir have been studied with a single 90 mg dose of ledipasvir in non-HCV infected patients with severe renal impairment (eGFR <30 mL / min by Cockcroft-Gault formula, median CrCl [limits] of 22 [17-29] mL / min). The pharmacokinetics of ledipasvir did not show any clinically significant difference between healthy subjects and patients with severe renal impairment.
- The pharmacokinetics of sofosbuvir have been studied in non-HCV-infected patients with mild (eGFR ≥ 50 and <80 mL / min / 1.73m 2 ), moderate (eGFR ≥ 30 and <50 mL / min / renal impairment ). 1.73 m 2 ), severe (eGFR <30 mL / min / 1.73 m 2 ) and in patients with ESRD requiring hemodialysis, after a single 400 mg dose of sofosbuvir. Compared with patients with normal renal function (eGFR> 80 mL / min / 1.73 m 2 ), the 0-inf AUC of sofosbuvir was 61%, 107% and 171% higher in mild renal impairment. moderate and severe, while AUC 0-infof GS-331007 was 55%, 88% and 451% higher, respectively. In patients with ESRD compared to patients with normal renal function, the AUC 0-inf of sofosbuvir was 28% higher when sofosbuvir was given 1 hour before hemodialysis, compared to 60% higher when sofosbuvir was given 1 hour after hemodialysis. ASC 0-infof GS-331007 in patients with ESRD who received sofosbuvir one hour before or one hour after hemodialysis was at least 10 and 20 times higher, respectively. GS-331007 is effectively removed by hemodialysis, with an extraction coefficient of approximately 53%. Following a single 400 mg dose of sofosbuvir, a 4 hour hemodialysis removed 18% of the administered sofosbuvir dose. The safety and efficacy of sofosbuvir have not been established in patients with severe renal impairment or ESRD.
Hepatic insufficiency
- The pharmacokinetics of ledipasvir have been studied with a single 90 mg dose of ledipasvir in non-HCV patients with severe hepatic impairment (CPT C score). Plasma exposure to ledipasvir (AUC inf ) was similar in patients with severe hepatic impairment and in control patients with normal hepatic function. Pharmacokinetic analysis of HCV-infected patient populations showed that cirrhosis has no clinically significant effect on exposure to ledipasvir.
- The pharmacokinetics of sofosbuvir were studied after 7 days of administration of 400 mg / day of sofosbuvir in HCV-infected patients with moderate or severe hepatic impairment (CPT scores B and C). Compared to patients with normal hepatic function, the AUC 0-24 of sofosbuvir was 126% and 143% higher, respectively, in moderate or severe hepatic impairment, while the AUC 0-24 of GS-331007 was 18% and 9% respectively higher. Population pharmacokinetic analysis in HCV infected patients has shown that cirrhosis has no clinically significant effect on exposure to sofosbuvir and GS-331007.
Body weight
- Body weight had no significant effect on exposure to sofosbuvir based on population pharmacokinetic analysis. Exposure to ledipasvir decreases with increased body weight, but this effect is not considered clinically significant.
Pediatric population
- The pharmacokinetics of ledipasvir, sofosbuvir and GS-331007 have not been established in children.
(see section Dosage and method of administration ).
harvoni treatment side effects
In addition to the desired effect, this can cause drug side effects.
The main side effects are the following.
Sometimes (from 10 to 30 people in 100)
- Headache , fatigue.
Rarely (from 1 to 10 in 100 people)
- Skin rash . Contact your doctor if you notice this.
Very rare (affects less than 1 in 100 people)
- Hypersensitivity to this medication. This can be expressed in ‘angioedema’: a swelling of the face, lips, mouth, tongue or throat. You can be very stuffy. If it occurs, you should immediately seek out a doctor or go to the First Aid Service. You can not use this type of medication in the future. Therefore tell the pharmacy that you are hypersensitive to this sofosbuvir with ledipasvir. The pharmacy team can then ensure that you do not get this medication again.
Consult your doctor if you suffer too much from one of the above mentioned side effects or if you experience other side effects that you are worried about.
harvoni interactions
Harvoni containing ledipasvir and sofosbuvir, all the interactions that have been observed with these active ingredients used individually can occur with Harvoni.
Potential effect of Harvoni on other drugs
Ledipasvir is an in vitro inhibitor of the P-gp drug transporter and Breast Cancer Resistance Protein (BCRP) protein and may increase the intestinal absorption of substrates from these transporters in case of co-infection. administration. In vitro data indicate that ledipasvir may be a weak inducer of metabolic enzymes such as CYP3A4, CYP2C and UGT1A1. Plasma concentrations of the compounds that are substrates of these enzymes could be reduced when co-administered with the ledipasvir / sofosbuvir combination. In vitro, ledipasvir inhibits intestinal CYP3A4 and UGT1A1. Drugs with a narrow therapeutic range and metabolized by these isoenzymes should be used with caution and under close supervision.
Potential effect of other drugs on Harvoni
Ledipasvir and sofosbuvir are substrates of the P-gp drug carrier and BCRP, whereas GS-331007 is not.
Drugs that are potent inducers of P-gp (rifampicin, rifabutin, St. John’s wort, carbamazepine, phenobarbital and phenytoin) can significantly decrease plasma concentrations of ledipasvir and sofosbuvir, reducing the therapeutic effect the ledipasvir / sofosbuvir association and therefore they are against-marked Harvoni (see Contraindications ). Drugs that are moderate inducers of P-gp in the gut (such as oxcarbazepine) may decrease plasma concentrations of ledispavir and sofosbuvir, reducing the therapeutic effect of Harvoni. Co-administration of this type of medication with Harvoni is not recommended (see section Warnings and Precautions section).). Co-administration of drugs that inhibit P-gp and / or BCRP may increase the plasma concentrations of ledipasvir and sofosbuvir without increasing that of GS-331007; Harvoni may be co-administered with inhibitors of P-gp and / or BCRP. No clinically significant effect on the ledipasvir / sofosbuvir combination is expected via CYP450 or UGT1A1 enzymes.
Patients treated with vitamin K antagonists
Because hepatic function may change during treatment with Harvoni, close monitoring of International Normalized Index (INR) values is recommended.
Interactions between Harvoni and other drugs
Table 3 provides a list of clinically established or potentially clinically significant drug interactions (where the 90% confidence interval [IC] of the mean geometric least squares ratio [GLSM] was within the “↔” limits, in excess of “↑ “, Or lower than” ↓ “predetermined equivalence limits). The drug interactions described are based on studies conducted either with the combination of ledipasvir / sofosbuvir or with ledipasvir and sofosbuvir taken individually, or are predictions of drug interactions that may occur with the combination of ledipasvir / sofosbuvir. This table is not exhaustive.
Harvoni Warnings and Precautions :
Harvoni should not be administered at the same time as other medicines containing sofosbuvir.
Activity according to genotype
- For recommended treatments for different genotypes of HCV, see Dosage and Method of Administration . For virologic and clinical activity by genotype, see the topic Pharmacodynamic properties .
- Clinical evidence supporting the use of Harvoni in patients with HCV genotype 3 is limited . The relative efficacy of 12-week treatment with ledipasvir / sofosbuvir + ribavirin compared to a 24-week course with sofosbuvir + ribavirin, has not been studied. A conservative treatment of 24 weeks is recommended in all previously treated genotype 3 patients and in patients who are naive to any treatment with cirrhosis (see Dosage and method of administration section ).
- Clinical evidence supporting the use of Harvoni in patients with HCV genotype 2 and 6 is limited.
- Severe Bradycardia and Conduction Disorders
- Cases of severe bradycardia and conduction disturbances have been observed with Harvoni when co-administered with amiodarone with or without other heart rate-lowering drugs. The mechanism is not established.
- The concomitant use of amiodarone has been limited in the clinical development of sofosbuvir in combination with direct-acting antivirals (DAAs). Some cases have been life-threatening. Therefore, amiodarone should be used in patients treated with Harvoni only in case of intolerance or contraindication to other anti-arrhythmic treatments.
- If concomitant use of amiodarone is considered necessary, close monitoring of patients is recommended when initiating Harvoni treatment. Patients identified as being at high risk for bradyarrhythmia should be monitored continuously for 48 hours in an adapted hospital environment.
- Given the long half-life of amiodarone, appropriate monitoring should also be performed in patients who have discontinued amiodarone in recent months and need to start treatment with Harvoni.
- All patients treated with Harvoni who receive amiodarone with or without other bradycardic medications should also be advised of symptoms of bradycardia and conduction disturbances, and should be informed of the need for urgent medical attention. feel these symptoms.
- Treatment of patients previously treated with direct-acting antivirals for HCV In patients who have failed treatment with ledipasvir / sofosbuvir, a selection of resistance mutations in NS5A significantly reduces susceptibility to ledipasvir.
- majority of cases (see section 5.1).). Limited data indicates that this type of mutation in NS5A is not reversible at long-term follow-up. In patients who have failed prior therapy with ledipasvir / sofosbuvir, there is currently no evidence to support the efficacy of re-treatment with NS5A inhibitor therapy. Similarly, in patients who have failed previous treatment with an NS3 / 4A protease inhibitor, there are currently no data supporting the efficacy of NS3 / 4A protease inhibitors. In these patients, the treatment of HCV infection may therefore depend on the use of other classes of drugs. Therefore, it will be necessary to
Renal failure
- No dose adjustment of Harvoni is required in patients with mild or moderate renal impairment. The safety of Harvoni has not been evaluated in patients with severe renal impairment (estimated glomerular filtration rate [eGFR] <30 mL / min / 1.73 m 2 ) or end-stage renal disease (IRT) requiring hemodialysis. If Harvoni is used in combination with ribavirin, also refer to the Summary of Product Characteristics of Ribavirin for patients with creatinine clearance (CrCl) <50 mL / min (see section 5.2 ).
- Patients with decompensated cirrhosis and / or waiting for liver transplantation or post-liver transplantation
- The efficacy of ledipasvir / sofosbuvir in patients with genotype 5 or genotype 6 HCV with decompensated cirrhosis and / or awaiting liver transplantation or post-liver transplantation has not been studied. The Harvoni treatment decision should be based on an assessment of the potential benefits and risks for each patient.
Use with moderate inducers of P-gp
Drugs that are moderate inducers of P-gp in the intestine (such as oxcarbazepine) may decrease the plasma concentrations of ledipasvir and sofosbuvir, reducing the therapeutic effect of Harvoni. Co-administration of this type of medication with Harvoni is not recommended (see section Interactions with other medicinal products and other forms of interaction ).
Use with some antiretrovirals for HIV
Harvoni has been shown to increase the exposure to tenofovir, particularly when used in combination with an HIV treatment containing tenofovir disoproxil fumarate and a pharmacokinetic booster (ritonavir or cobicistat). The safety of tenofovir disoproxil fumarate in the context of Harvoni treatment in the presence of a pharmacokinetic booster has not been established. The potential risks and benefits associated with co-administration of Harvoni with the fixed-dose combination tablet containing elvitegravir / cobicistat / emtricitabine / tenofovir disoproxil fumarate or tenofovir disoproxil fumarate used in combination with a protease inhibitor Boosted HIV (eg atazanavir or darunavir) should be considered, especially in patients at increased risk of renal dysfunction. In patients receiving concomitant Harvoni with elvitegravir / cobicistat / emtricitabine / tenofovir disoproxil fumarate or with tenofovir disoproxil fumarate and a boosted HIV protease inhibitor, undesirable effects associated with tenofovir should be monitored. See the Summary of Product Characteristics for tenofovir disoproxil fumarate, emtricitabine / tenofovir disoproxil fumarate, or elvitegravir / cobicistat / emtricitabine / tenofovir disoproxil fumarate for recommendations for monitoring renal function. elventegravir / cobicistat / emtricitabine / tenofovir disoproxil fumarate or with tenofovir disoproxil fumarate and a boosted HIV protease inhibitor, undesirable effects associated with tenofovir should be monitored. See the Summary of Product Characteristics for tenofovir disoproxil fumarate, emtricitabine / tenofovir disoproxil fumarate, or elvitegravir / cobicistat / emtricitabine / tenofovir disoproxil fumarate for recommendations for monitoring renal function. elventegravir / cobicistat / emtricitabine / tenofovir disoproxil fumarate or with tenofovir disoproxil fumarate and a boosted HIV protease inhibitor, undesirable effects associated with tenofovir should be monitored. See the Summary of Product Characteristics for tenofovir disoproxil fumarate, emtricitabine / tenofovir disoproxil fumarate, or elvitegravir / cobicistat / emtricitabine / tenofovir disoproxil fumarate for recommendations for monitoring renal function.
Use with HMG-CoA reductase inhibitors
Co-administration of Harvoni with HMG-CoA reductase inhibitors (statins) can significantly increase the statin concentration, increasing the risk of myopathy and rhabdomyolysis (see section 4.5). forms of interactions ).
HCV / HBV co-infection (hepatitis B virus)
Cases of hepatitis B virus (HBV) reactivation, some with fatal outcome, have been reported during or after treatment with direct-acting antiviral agents. HBV testing should be performed in all patients prior to initiation of treatment. Patients co-infected with HBV / HCV are at risk for reactivation of HBV and should therefore be monitored and managed according to clinical guidelines.
Pediatric population
- Harvoni is not recommended for use in children and adolescents under 18 years of age as the safety and efficacy of this medication have not been established in this population.
excipients
- Harvoni contains an azo dye, S Yellow Orange Lake (E110), which can cause allergic reactions. It also contains lactose. As a result, patients with rare hereditary problems of galactose intolerance, Lapp lactase deficiency or glucose / galactose malabsorption should not take this medicine.
Drive and use machines
Harvoni (alone or in combination with ribavirin) has no or negligible effect on the ability to drive and use machines.
However, patients should be informed that fatigue was more common in patients treated with ledipasvir / sofosbuvir than in those receiving placebo.
Harvoni and PREGNANCY / BREAST FEEDING / FERTILITY
Women of childbearing
- potential / contraception in men and women When Harvoni is used in combination with ribavirin, all precautions should be taken to prevent pregnancy in patients and female partners of patients. Significant teratogenic and / or embryocidal effects have been demonstrated in all animal species exposed to ribavirin. Women of childbearing potential or their male partners should use an effective method of contraception during treatment and for some time after the end of treatment, as recommended in the Summary of Product Characteristics of Ribavirin.
- See the Summary of Product Characteristics of Ribavirin for more information.
Pregnancy
- There are no data or limited data (less than 300 pregnancies) on the use of ledipasvir, sofosbuvir or Harvoni in pregnant women.Studies in animals have not shown any direct deleterious effects on reproduction. No significant effects on fetal development were observed in rats and rabbits with ledipasvir or sofosbuvir. However, it was not possible to completely evaluate margins of exposure with sofosbuvir in rats in relation to human exposure at the recommended clinical dose.
- As a precaution, it is best to avoid the use of Harvoni during pregnancy.
feeding
- It is not known whether ledipasvir or sofosbuvir and their metabolites are excreted in breast milk.The pharmacokinetic data available in animals have demonstrated the excretion of ledipasvir and metabolites of sofosbuvir in milk
- A risk for newborns / infants can not be ruled out. Therefore, Harvoni should not be used while breastfeeding.
Fertility
There is no data on the effect of Harvoni on human fertility. Studies in animals have not shown deleterious effects of ledipasvir or sofosbuvir on fertility.
If ribavirin is co-administered with Harvoni, contraindications for the use of ribavirin during pregnancy and lactation apply (see also Summary of Product Characteristics of Ribavirin).
What should I do if I miss a dose?
It is important to take this medicine consistently. If you have forgotten a dose:
You use this medicine once a day:
- Does it take more than 6 hours before you should take the next dose? Swallow the forgotten tablet as soon as
- possible and take the next dose at the usual time.
- Does it take less than 6 hours before you should take the next dose? Skip the forgotten tablet and take the next dose at the usual time.
What happens if I overdose from Harvoni ?
The highest documented doses of ledipasvir and sofosbuvir were 120 mg twice daily for 10 days and 1200 mg once, respectively. In these studies in healthy volunteers, no adverse events were observed at these doses and the adverse effects were similar in frequency and intensity to those reported in the placebo groups. The effects of higher doses are not known.
There is no specific antidote for overdose of Harvoni. If overdose occurs, all symptoms of toxicity will be monitored in the patient. Treatment of Harvoni overdose consists of general supportive measures, with monitoring of vital signs and observation of the patient’s clinical condition. It is unlikely that hemodialysis will significantly eliminate ledipasvir since ledipasvir is highly bound to plasma proteins. Hemodialysis can effectively remove the main circulating metabolite of sofosbuvir (ie GS-331007), with a 53% extraction ratio.
What is Forms and Composition Harvoni?
90 mg / 400 mg film-coated tablet (diamond shaped, orange, size 19 mm × 10 mm, on one side with “GSI” inscription and on the other side “7985”): Bottle of 28, with child safety closure system.
NOT’s
Edrug-online contains comprehensive and detailed information about drugs available in the medical field, and is divided into four sections:
general information:
- Includes a general description of the drug, its use, brand names, FAQs, and relevant news and articles
Additional information:
- General explanation about dealing with the medicine: how to take the medicine, the doses and times of it, the start and duration of its effectiveness, the recommended diet during the period of taking the medicine, the method of storage and storage, recommendations in cases for forgetting the dose and instructions to stop taking the drug and take additional doses.
Special warnings:
- For pregnant and breastfeeding women, the elderly, boys and drivers, and use before surgery.
Side effects:
- It treats possible side effects and drug interactions that require attention and its effect on continuous use.
- The information contained in this medicine is based on medical literature, but it is not a substitute for consulting a doctor.
The post Harvoni medication Uses, Dosage, Side Effects, Precautions & Warnings appeared first on Drug Online.
from Drug Online
https://bit.ly/3eY6utB
via Edrug Online
Comments
Post a Comment